Table of Contents
ToggleIntroduction
CPAP vs. BiPAP—Which one is right for you?. Sleep apnea and other respiratory disorders can significantly affect your quality of life. People with sleep apnea experience pauses in breathing while sleeping, leading to poor sleep quality, daytime fatigue, and serious health risks.
The two most common treatments for sleep apnea are CPAP (Continuous Positive Airway Pressure) and BiPAP (Bilevel Positive Airway Pressure). But what’s the difference between them, and how do you know which one is right for you? In this guide, we’ll break down the details, benefits, and key differences between CPAP and BiPAP machines.
What Is CPAP?

Definition of CPAP (Continuous Positive Airway Pressure)
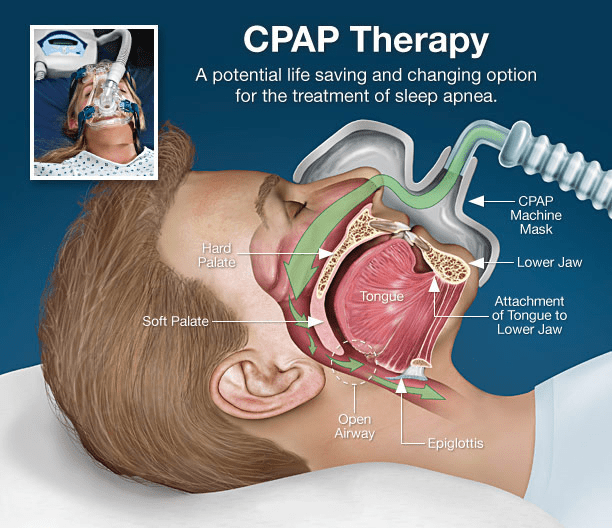
A CPAP machine is a medical device that delivers a constant and steady flow of air through a mask to keep the airway open during sleep. It is the most common treatment for obstructive sleep apnea (OSA) and helps prevent airway collapse.
How CPAP Works
A CPAP machine consists of the following components:
- A motorized air pump that provides a constant stream of air
- A mask that fits over your nose or mouth
- A tube that connects the mask to the machine
The machine pushes air into your airway at a fixed pressure, preventing blockages and ensuring normal breathing patterns while you sleep. This shows the difference between CPAP vs. BiPAP—Which one is right for you
Who Needs CPAP Therapy?
CPAP therapy is recommended for individuals with:
✅ Obstructive sleep apnea (OSA)
✅ Snoring and breathing interruptions during sleep
✅ Fatigue and daytime sleepiness due to poor sleep
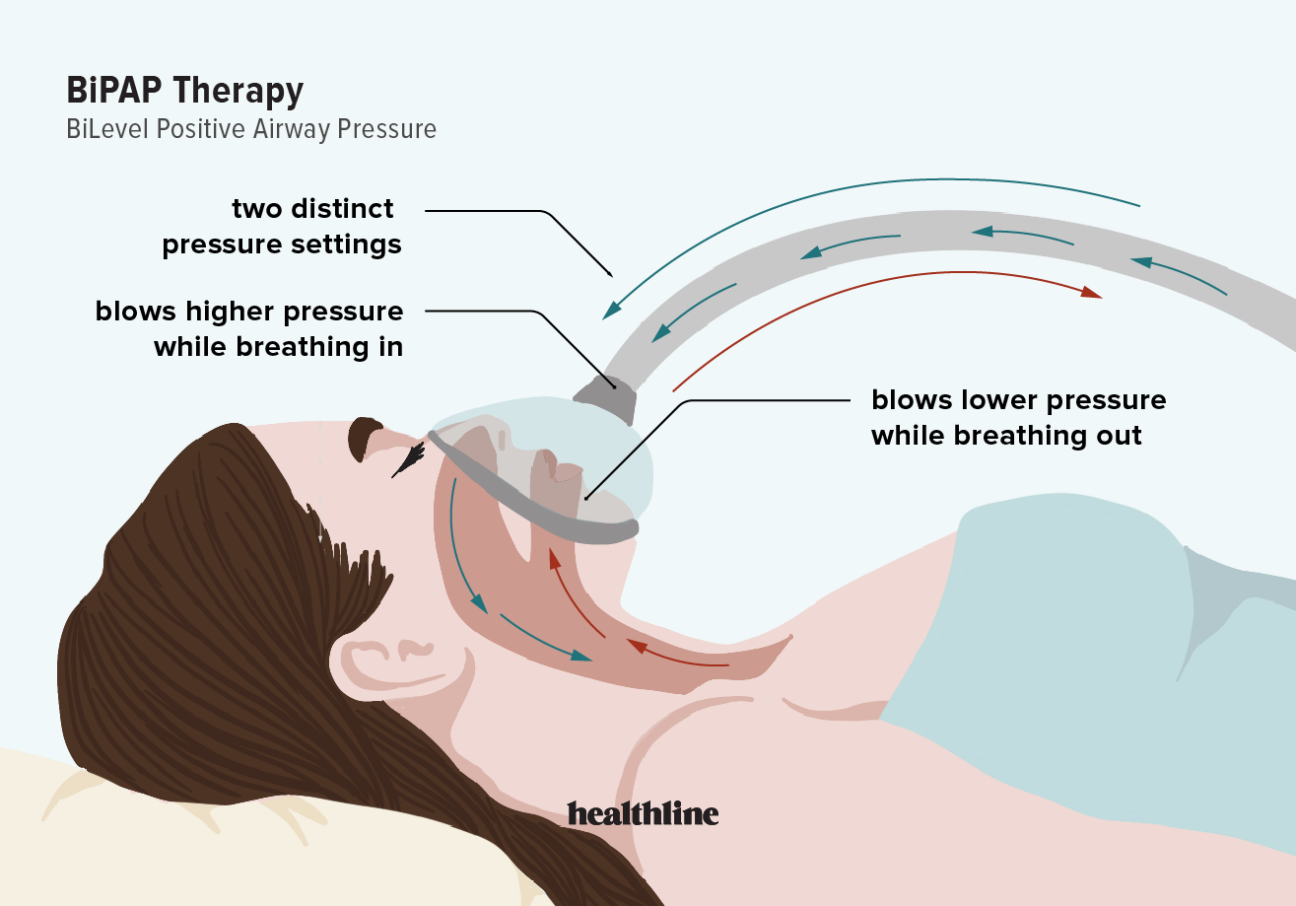
What Is BiPAP?

Definition of BiPAP (Bilevel Positive Airway Pressure)
A BiPAP machine works similarly to CPAP but delivers two different levels of air pressure:
- Higher pressure for inhalation (IPAP)
- Lower pressure for exhalation (EPAP)
This dual-level pressure makes it easier for people with certain breathing disorders to breathe more comfortably.
How BiPAP Works
The BiPAP machine adjusts pressure levels based on whether you are inhaling or exhaling. This allows for a more natural breathing process, especially for people with respiratory conditions that make exhalation difficult. This shows the difference between CPAP vs. BiPAP—Which one is right for you
Who Needs BiPAP Therapy?
BiPAP therapy is often prescribed for patients with:
✅ Central sleep apnea (CSA)
✅ Chronic obstructive pulmonary disease (COPD)
✅ Neuromuscular disorders
✅ Congestive heart failure
Key Differences Between CPAP and BiPAP
| Feature | CPAP | BiPAP |
|---|---|---|
| Pressure Type | Single continuous pressure | Two pressure levels (inhale & exhale) |
| Best for | OSA patients | CSA, COPD, severe apnea |
| Comfort Level | May feel harder to exhale | More natural breathing pattern |
| Cost | Generally lower | More expensive |
| Insurance Coverage | Widely covered | May require special approval |
How CPAP Works: The Science Behind It
A CPAP machine maintains a continuous, constant pressure to keep your airway open while you sleep. The pressure setting is determined by a sleep study conducted by a doctor.
Many users find it uncomfortable at first, particularly when exhaling against a constant air pressure. However, newer CPAP models include ramp features that start at a lower pressure and gradually increase for comfort. This shows the difference between CPAP vs. BiPAP—Which one is right for you
How BiPAP Works: A Closer Look
Unlike CPAP, BiPAP machines adjust their pressure during inhalation and exhalation:
- IPAP (Inspiratory Positive Airway Pressure): Higher pressure to help inhale
- EPAP (Expiratory Positive Airway Pressure): Lower pressure to make exhalation easier
BiPAP is often used for patients who find CPAP uncomfortable or have additional respiratory complications. This shows the difference between CPAP vs. BiPAP—Which one is right for you
Pros and Cons of CPAP Therapy
Pros
✅ Effective for OSA
✅ More affordable than BiPAP
✅ Widely available
Cons
❌ Can feel uncomfortable due to continuous pressure
❌ Some users struggle with exhalation
Pros and Cons of BiPAP Therapy
Pros
✅ Easier breathing with two pressure levels
✅ Recommended for severe respiratory conditions
✅ More comfortable for some patients
Cons
❌ More expensive
❌ Requires doctor approval for insurance coverage
Which One Is Right for You?
- If you have mild to moderate OSA, CPAP is typically the best choice.
- If you struggle to exhale against CPAP pressure or have more complex breathing conditions, BiPAP may be better.
- A sleep study and doctor’s recommendation will help determine the best option.
This shows the difference between CPAP vs. BiPAP—Which helps to choose right for you
Cost Comparison: CPAP vs. BiPAP
| Machine Type | Average Cost | Insurance Coverage |
|---|---|---|
| CPAP | $500 – $1,500 | Widely covered |
| BiPAP | $1,500 – $3,000 | Requires medical necessity approval |
Maintenance and Cleaning Tips
- Daily: Wipe mask and clean tubing.
- Weekly: Wash mask, humidifier, and replace filters.
- Monthly: Check for wear and tear on the mask and tubing.
Common Myths & Misconceptions About CPAP and BiPAP
- ❌ “BiPAP is just a more expensive CPAP” – No, BiPAP is designed for specific conditions.
- ❌ “I don’t need to clean my CPAP/BiPAP often” – Regular cleaning prevents infections.
- ❌ “CPAP is only for older people” – Sleep apnea affects all ages.
Conclusion
Choosing between CPAP and BiPAP depends on your specific condition. If you have obstructive sleep apnea, CPAP is often the first choice. However, if you have central sleep apnea, COPD, or need additional breathing support, BiPAP may be more suitable. This shows the difference between CPAP vs. BiPAP—Which one is right for you
FAQ's
Can CPAP be used instead of BiPAP?
CPAP works for most OSA patients, but BiPAP is better for those with more complex respiratory issues.
Is BiPAP better for severe sleep apnea?
Yes, BiPAP is more effective for severe cases or patients who struggle with CPAP.
How long does it take to get used to CPAP/BiPAP?
It varies, but most people adjust within 1-2 weeks.
Does insurance cover BiPAP machines?
Yes, but only if medically necessary.
What happens if I don’t use my CPAP/BiPAP regularly?
You may experience worsened symptoms, poor sleep, and increased health risks.